Find Out When You Can Switch Medicare Advantage Plans
If there is one constant in life, it's change. And if your medical needs or living circumstances change, so should your healthcare coverage.
Speak with a Medicare Advocate
Medicare helps you adapt. It lets you switch health insurance plans at specific times each year.
Keep reading to find out when you can change your Medicare Advantage plan and how to qualify for Special Enrollment Periods.
Can I Change My Medicare Advantage Plan?
Yes!
If you're unhappy with your current plan or want to change your coverage, you can switch from one Medicare Advantage Plan to another, or return to Original Medicare. However, there are exceptions to when you can switch plans.
Note: Before switching plans, compare the costs
When Can I Change My Medicare Advantage Plan?
You can join, change, or drop your Medicare Advantage plan during these specific periods:
Initial Enrollment period
Annual Election Period
Medicare Advantage Open Enrollment Period
Let's look at each period in detail.
Initial Enrollment Period
You first sign up for Medicare during the Initial Enrollment period.
You start by enrolling in Parts A and B. Then, you can switch to any Medicare Advantage plan of your choice.
Your Initial enrollment period (IEP)
Below are some examples:
You’re Eligible as Soon as You Turn 65
Your IEP is a 7-month window:
It begins 3 months before you turn 65.
It ends 3 months after your birth month.
If you enroll in a Medicare Advantage Plan during this time and aren't satisfied, you can drop it anytime within the next 12 months and return to Original Medicare.
You’re Eligible Due to a Disability (And You're Under 65)
Your IEP is a 7-month window:
It begins 3 months before your Medicare coverage begins (24 months after you get Social Security or RRB benefits)
It extends to 3 months after you start getting Medicare benefits
You’re Eligible Due to a Disability (and You Turn 65)
Your IEP is a 7-month window:
It begins 3 months before you turn 65.
It ends 3 months after your birth month.
During this period, you can either join, drop, or switch your Medicare Advantage Plan.
You Have Medicare Part A and Get Part B During the General Enrollment Period
If you add Medicare Part B during the GEP (January 1st – March 31st), your IEP lasts from April 1st – June 30th.
Annual Election Period
The Annual Election Period (AEP) also known as the Fall Open Enrollment occurs from October 15th – December 7th each year.
During this period, you can:
Switch from Original Medicare to Medicare Advantage Plan.
Return to Original Medicare from a Medicare Advantage Plan.
Switch from one Medicare Advantage Plan to another (with or without drug plans).
Join a Medicare drug plan (Part D).
Switch from one Medicare drug plan to another.
Disenroll from a Medicare drug coverage.
Changes made during the AEP come into effect on January 1st.
Medicare Advantage Open Enrollment Period
The Medicare Advantage Open Enrollment Period (MA OEP) occurs from January 1st – March 31st each year.
During this period, you can:
Switch from a Medicare Advantage Plan to another plan
Return to Original Medicare from a Medicare Advantage Plan
However, you can’t:
Switch from Original Medicare to the Medicare Advantage Plan
Join a Medicare drug plan (Part D)
Switch from one Medicare drug plan to another
The change made during the MA OEP comes into effect the first of the month following enrollment.
Note: you can only switch your plan once during this period.
Can You Change Medicare Advantage Plans at Any Other Time?
Yes. You can switch plans outside the three enrollment periods.
To do this, you must qualify for the Special Enrollment Period (SEP).
You're eligible for the Special Enrollment Period if:
You move to a different location
You lose your current coverage
You have a chance to get other coverage
Your plan changes its contract with Medicare
The state you live in grants an SEP
Let's look at some specific situations in more detail and discuss some steps you can take.
1. Your Change of Address Affects Your Coverage
If you move to a new address outside your plan's service area or your original service provider introduces plan options in your new location, you can:
Switch to a new Medicare Advantage plan or Medicare drug plan
Return to Original Medicare (if you’re outside your plan’s service area)
Note: If you don’t enroll in a new Medicare Advantage plan, you’ll automatically get Original Medicare when you disenroll from your old MA plan.
How Long Is the Special Enrollment Period?
If you inform your service provider before you move — your SEP begins the month before you move and extends to 2 months after you move.
If you inform your service provider after you move — your SEP starts the month you tell your provider and ends after 2 months.
2. You Move Back to the United States
If you leave the U.S. and move back, you can join a Medicare Advantage Plan or a Medicare drug plan.
How Long Is the Special Enrollment Period?
Your SEP lasts from 1 month before you move until 2 months after you move back to the U.S.
3. You Move Out of an Institution
If you recently moved out of a nursing home or rehabilitation hospital, you can:
Join a Medicare Advantage Plan or Medicare drug plan.
Switch from your current plan to another Medicare Advantage Plan or Medicare drug plan.
Return to Original Medicare.
Drop your Medicare drug coverage.
How Long Is the Special Enrollment Period?
Your SEP lasts as long as you live in the institution. It ends 2 months after you move out.
4. You're No Longer Eligible for Medicaid
If you no longer qualify for Medicaid, you can:
Join a Medicare Advantage Plan or Medicare drug plan
Switch from your current plan to another Medicare Advantage Plan or Medicare drug plan
Return to Original Medicare
Drop your Medicare drug coverage
How Long Is the Special Enrollment Period?
Your SEP lasts for 3 months from whichever date is later:
The date you’re no longer eligible
The date you find out you’re no longer eligible
5. You Lose Coverage With Your Employer
If your employer or union no longer provides coverage (including COBRA coverage), you can join a Medicare Advantage Plan or Medicare drug plan.
How Long Is the Special Enrollment Period?
Your SEP lasts for 2 months after your coverage ends or 2 months after you are notified, whichever is later.
6. You're Impacted by Medicare Exclusions
If Medicare takes an official action (a “sanction”) because of a problem with the plan, you can switch from your Medicare Advantage Plan or Medicare drug plan to another plan.
How Long Is the Special Enrollment Period?
Medicare determines your SEP on a case-by-case basis.
7. Your Plan Terminates Its Contract with Medicare
If your plan is no longer part of Medicare, you can switch from your Medicare Advantage Plan or Medicare drug plan to another plan.
How Long Is the Special Enrollment Period?
Your SEP begins 2 months before the contract ends and extends till one month after.
8. Your Plan Isn't Renewed
If your Medicare Advantage plan, Medicare drug plan, or Medicare Cost Plan isn’t renewed for the next contract year, you can switch from your Medicare Advantage Plan or Medicare drug plan to another plan.
How Long Is the Special Enrollment Period?
Your SEP acts as an extension of the AEP and starts on October 15th and ends on the last day of February.
9. You're Eligible for Both Medicare and Medicaid
If you qualify for both Medicare and Medicaid, you can:
Join a Medicare Advantage Plan or Medicare drug plan
Switch from your current plan to another Medicare Advantage Plan or Medicare drug plan
Return to Original Medicare
Drop your Medicare drug coverage
How Long Is the Special Enrollment Period?
You can join, switch, or drop once during each of these periods:
January – March
April – June
July – September
10. You Drop Medigap and Join Medicare Advantage
If you switch from Medigap to Medicare Advantage, you can:
Drop your Medicare Advantage Plan and enroll in Original Medicare
Buy a Medigap policy (with special rights)
How Long Is the Special Enrollment Period?
Your SEP lasts 12 months after you first join a Medicare Advantage Plan.
Other Situations
Some other special circumstances list
Takeaway
You may want to change or drop your Medicare Advantage Plan if:
You're unhappy with your current plan
Your doctor moves out of network
You move to a new place
Your medical situation changes
Whatever the case, Medicare lets you switch plans during specific enrollment periods.
You may also qualify for a Special Enrollment Period. Call Medicare or talk to our licensed advisors at 1-888-376-2028 to check your eligibility.
If switching plans feels confusing, Fair Square Medicare
Recommended Articles

Does Medicare Cover the WATCHMAN Procedure?
Dec 1, 2022

How Often Can I Change Medicare Plans?
May 5, 2023
Can Medicare Advantage Plans Deny Coverage for Pre-Existing Conditions?
Mar 28, 2023

13 Best Ways for Seniors to Stay Active in Phoenix
Mar 6, 2023

Do I Need Medicare If My Spouse Has Insurance?
Dec 19, 2022

Last Day to Change Your Medicare Part D Plan
Jul 14, 2025

Does Medicare Cover Cartiva Implants?
Nov 29, 2022

Does Medicare Cover RSV Vaccines?
Sep 13, 2023

Does Medicare Cover Cold Laser Therapy (CLT)?
Jun 14, 2023

Is HIFU Covered by Medicare?
Nov 21, 2022
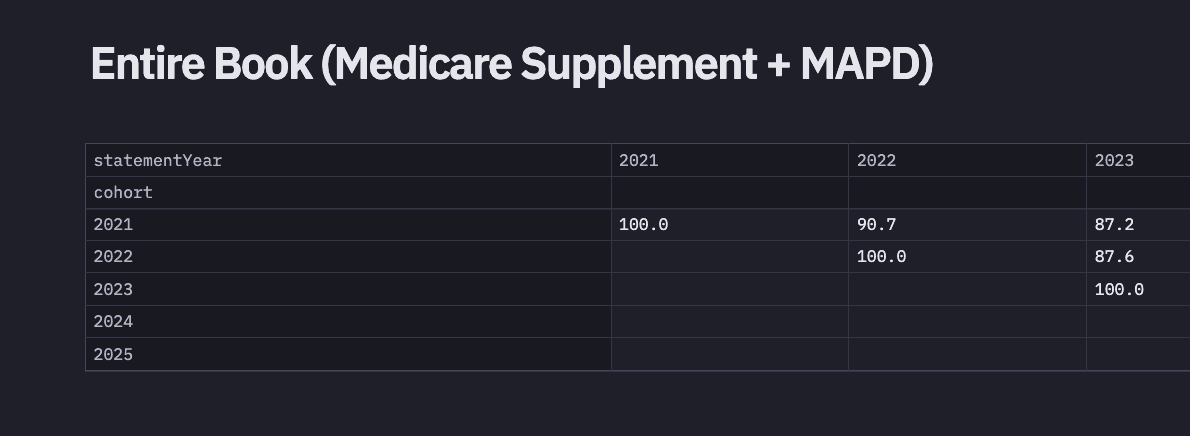
2024 Fair Square Client Retention and Satisfaction Report
Mar 4, 2025

Medicare 101
May 20, 2020

What is Plan J?
Jul 14, 2025

Is Emsella Covered by Medicare?
Nov 21, 2022
How to Enroll in Social Security
Apr 28, 2023

Does Medicare Cover Diabetic Eye Exams?
Jan 11, 2023
Does Medicare Cover Cardiac Ablation?
Dec 9, 2022

How to Compare Medigap Plans in 2025
Jul 14, 2025
More of our articles
10 Top Medicare Supplement (Medigap) Companies for 2025
13 Best Ways for Seniors to Stay Active in Philadelphia
2024 Cost of Living Adjustment
2025 Medicare Price Changes
Building the Future of Senior Healthcare
Can I Choose Marketplace Coverage Instead of Medicare?
Can I Have Two Primary Care Physicians?
Can Medicare Advantage Plans be Used Out of State?
Comparing All Medigap Plans | Chart Updated for 2025
Do All Hospitals Accept Medicare Advantage Plans?
Does Medicare Cover a Spinal Cord Stimulator?
Does Medicare Cover Abortion Services?
Does Medicare Cover an FMT?
Does Medicare Cover Breast Implant Removal?
Does Medicare Cover Cosmetic Surgery?
Does Medicare Cover COVID Tests?
Does Medicare cover Deviated Septum Surgery?
Does Medicare Cover Driving Evaluations?
Does Medicare Cover Hepatitis C Treatment?
Does Medicare Cover Hypnotherapy?
Does Medicare Cover Inqovi?
Does Medicare Cover Iovera Treatment?
Does Medicare Cover Jakafi?
Does Medicare Cover Krystexxa?
Does Medicare Cover Mental Health?
Does Medicare Cover Mouth Guards for Sleep Apnea?
Does Medicare Cover Nuedexta?
Does Medicare Cover Oxybutynin?
Does Medicare Cover Penile Implant Surgery?
Does Medicare Cover Physicals & Blood Work?
Does Medicare Cover Robotic Surgery?
Does Medicare Cover Scleral Lenses?
Does Medicare Cover Service Animals?
Does Medicare Cover SIBO Testing?
Does Medicare Cover the Urolift Procedure?
Does Medicare Cover Tymlos?
Does Medicare Cover Vitamins?
Does Medicare Cover Zilretta?
Does Medicare Have Limitations on Hospital Stays?
Does Medicare Pay for Funeral Expenses?
Does Medicare pay for Opdivo?
Does Medicare Require a Referral for Audiology Exams?
Does Your Medicare Plan Cover B12 Shots?
Everything About Your Medicare Card + Medicare Number
Explaining IRMAA on Medicare
Explaining the Different Enrollment Periods for Medicare
Finding the Best Dental Plans for Seniors
Finding the Best Vision Plans for Seniors
Gap Health Insurance: The Secret Sidekick to Your High-Deductible Plan
Health Savings Accounts (HSAs) and Medicare
How Are Medicare Star Ratings Determined?
How Do I Sign up for Medicare? A Simple How-To Guide For You
How Do Medigap Premiums Vary?
How Much Does Medicare Cost?
How Much Does Trelegy Cost with Medicare?
How to Apply for Medicare?
How to Choose a Medigap Plan
Is Balloon Sinuplasty Covered by Medicare?
Is Vitrectomy Surgery Covered by Medicare?
Medicare Deductibles Resetting in 2025
Medicare Explained
Medicare Supplement Plans for Low-Income Seniors
Medigap Plan N vs. Plan G — Which One Fits You in 2025?
Moving? Here’s What Happens to Your Medicare Coverage
Seeing the Value in Fair Square
The Fair Square Bulletin: October 2023
Top 10 Physical Therapy Clinics in San Diego
What Is a Medicare Supplement SELECT Plan?
What's the Difference Between HMO and PPO Plans?
When to Choose Medicare Advantage over Medicare Supplement
Why Is Medicare So Confusing?
Will Medicare Cover Dental Implants?
Get the Fair Square Bulletin
Medicare savings tips, helpful guides, and more.
Virgil Insurance Agency, LLC (DBA Fair Square Medicare) and www.fairsquaremedicare.com are privately owned and operated by Help Button Inc. Medicare supplement insurance plans are not connected with or endorsed by the U.S. government or the federal Medicare program. This is a solicitation of insurance. A licensed agent/producer may contact you. Medicare Supplement insurance is available to those age 65 and older enrolled in Medicare Parts A and B and, in some states, to those under age 65 eligible for Medicare due to disability or End-Stage Renal disease. Virgil Insurance Agency is a licensed and certified representative of Medicare Advantage HMO, HMO SNP, PPO, PPO SNP and PFFS organizations and stand-alone PDP prescription drug plans. Each of the organizations we represent has a Medicare contract. Enrollment in any plan depends on contract renewal. The plans we represent do not discriminate on the basis of race, color, national origin, age, disability, or sex. Plan availability varies by region and state. For a complete list of available plans please contact 1-800-MEDICARE (TTY users should call 1-877-486-2048), 24 hours a day/7 days a week or consult www.medicare.gov. © 2026 Help Button Inc
We do not offer every plan available in your area. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options.
MULTIPLAN_FairSquareMedicare_01062022_M
Fair Square Medicare


